In a state with low population density and where over half the population is considered to be living in a rural area, it is not surprising that individuals in Montana who are highest risk for a fatality due to a drug overdose might not be able to access suitable treatment programs. This access may be limited by geography, hesitancy to seek out help or visit a clinic in areas where “everyone knows each other,” or lack of awareness about treatment options. With these limiting factors in mind, the JG team used spatial analysis and qualitative research methods to inform an investigation on the feasibility of establishing mobile opioid treatment programs (OTP) in Montana.
The availability of medication for opioid use disorder (MOUD) by way of a mobile unit is a relatively novel concept. Widespread adoption was made practical in the past year due to the Drug Enforcement Agency (DEA) ruling on June 28, 2021, which eased restrictions on the transport of medications for treating opioid use disorder (OUD). It is now much simpler and more streamlined for mobile units to deliver methadone or buprenorphine to rural areas that otherwise have limited to no access to treatment.
THIS STUDY HAS TWO PRIMARY GOALS:
- Complete a feasibility assessment to inform planning and strategy for mobile van unit implementation in Montana.
- Document current practices among existing mobile units to inform planning processes
A spatial analysis of areas of greatest need was conducted in order to find potential routes for a mobile OTP. Greatest need areas were determined as counties that have little or no access to MOUD providers but are still seeing high rates of opioid overdoses. The following figures show the proposed travel routes to these underserved populations in western and northwest Montana.
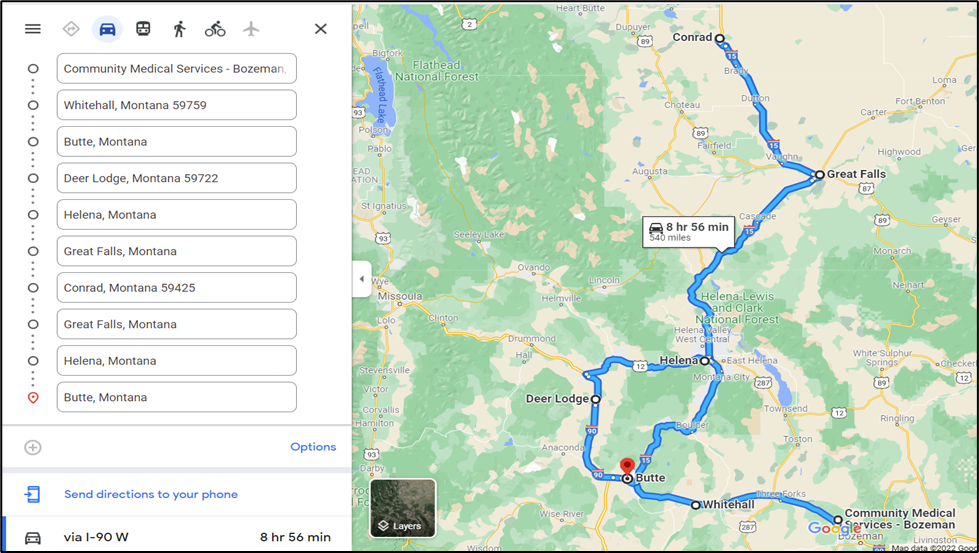
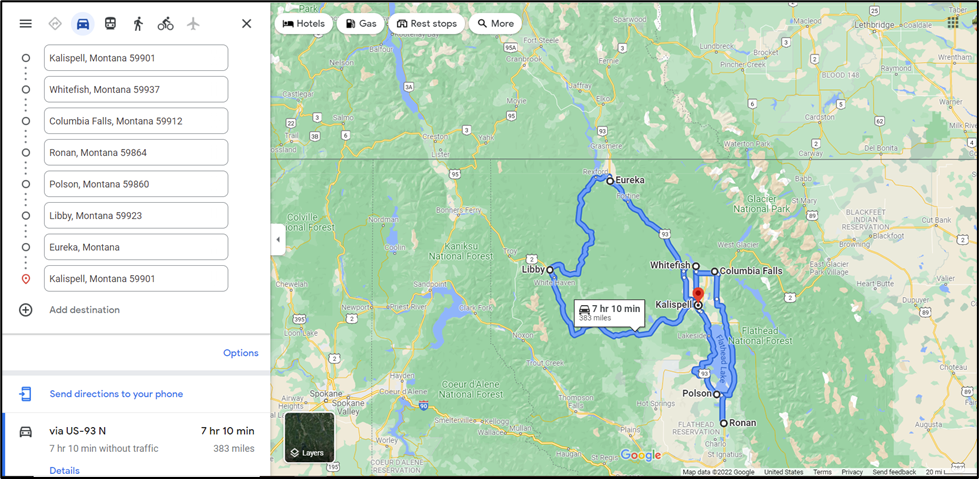
The next step in selecting the best route for a mobile OTP is determining a prioritization schema for which populations should be served, and determining how long the mobile unit should stay in each location. Once the general route is decided, parking locations can be explored and publicized.
Key findings of the feasibility study:
- Suspected overdoses tend to be clustered in population centers in Montana that have existing opioid treatment services. There is evidence that additional services and innovative approaches may be needed in these areas to engage at-risk populations in treatment programs.
- Key stakeholders interviewed in Montana are generally supportive of additional services being provided to treat OUD in the form of a mobile unit and recognize this as a potentially innovative solution to under engagement in MOUD treatment.
- Experienced mobile OTP providers identified community education as the most important piece to successful implementation of mobile OTP services. Educational efforts should include details about mobile OTP as well as a direct discussion of stigma directed towards people who use drugs and towards addiction.
- Experts in implementing and running mobile units identified practical concerns related to funding, billing, and workflow that can be used to guide mobile OTP service implementation.
This report was written by Karl Vanderwood, PhD, Grace Stonecipher, MS, Sue Myers, MPH, and Brandn Green, PhD (JG Research & Evaluation) for the Behavioral Health and Development Disabilities Division (BHDD) of the Montana Department of Health and Human Services (DPHHS). Funding for this study was provided by BHDD through the Substance Abuse and Mental Health Services Administration (SAMHSA) State Opioid Response II grant program. The Montana Public Health Institute provided grant management and support for this study.
To read the full report, follow this link to the JG publications page.